Are you sick of browsing through stale magazines in congested waiting areas while you wait for your doctor’s appointment? Well, fear not, telemedicine has arrived! Telemedicine, which uses technology to deliver healthcare remotely, has been causing a stir in the healthcare sector for a while. In fact, recent developments in telemedicine in the USA have fundamentally changed how healthcare is provided.
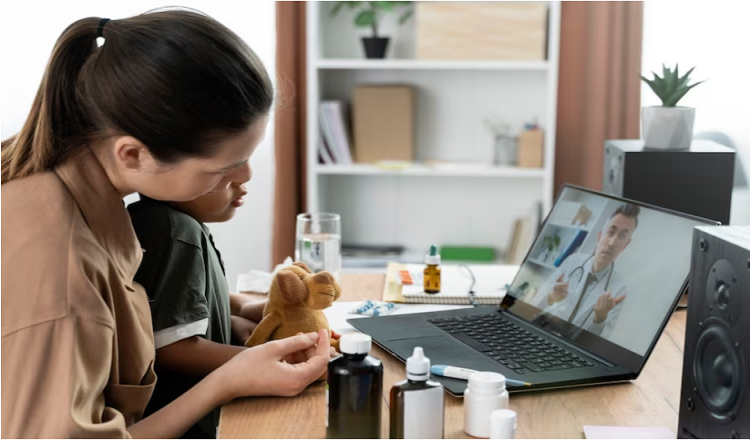
What precisely is telemedicine, you ask? In essence, it enables patients to digitally communicate with healthcare professionals via video conferencing, messaging, or other online platforms. This implies that you might obtain medical guidance, a diagnosis, or even a prescription filling without ever leaving your home! One of telemedicine’s most important benefits, particularly for people who live in isolated or underdeveloped locations, is convenience.
The COVID-19 epidemic has made the value of telemedicine in healthcare even more clear. Due to social isolation policies, many people have been forced to rely on telemedicine to access essential medical care. Telemedicine, however, is not a novel idea; in fact, it has a long history in the United States. So let’s go back in time and examine the development of telemedicine in the USA as well as the most recent innovations that are reshaping the face of healthcare as we know it.
Remote patient observation
With the use of technology, healthcare professionals can watch patients using remote patient monitoring (RPM), a type of telemedicine. It calls for the use of gadgets and sensors that gather and send information about the patient, including vital signs, blood glucose levels, and medication compliance. Wearable fitness trackers, smart watches, blood glucose monitors, and blood pressure cuffs are a few examples of RPM devices. Following collection, the data is sent to healthcare professionals for analysis and, if necessary, intervention.
RPM has many advantages in telemedicine. It enables medical professionals to monitor patients’ health state in real-time and take the appropriate action before a condition worsens. RPM also gives medical professionals the ability to remotely manage chronic diseases like diabetes and hypertension, which eliminates the need for repeated in-person visits. RPM has also been demonstrated to lower healthcare expenditures, decrease readmissions to hospitals, and enhance patient outcomes. RPM is a strong instrument that enhances patient care and boosts healthcare delivery effectiveness overall.
Telemedicine with artificial intelligence (AI)
An developing technology called artificial intelligence (AI) has the potential to completely transform the healthcare sector, including telemedicine. AI in telemedicine refers to the use of clever algorithms and software to help doctors diagnose, treat, and manage patients at a distance. Computer-aided diagnostics, chatbots, and virtual nursing assistants are a few examples of AI applications in telemedicine.
Numerous advantages of AI in telemedicine include enhanced effectiveness, quicker turnaround times, and improved diagnostic and therapeutic accuracy. However, there are drawbacks to using AI in telemedicine, including worries about data security and privacy as well as the possibility of bias in the algorithms. Overall, telemedicine’s usage of AI has the potential to raise patient access to healthcare services while also improving the quality of care.
Technology for Wearables in Telemedicine
Smartwatches and fitness trackers are common examples of wearable technology, which is a category of electronic gadget that can be worn on the body and collects and transmits data on a person’s activity and health. Wearable technology has the potential to be a game-changer in telemedicine by enabling real-time patient tracking and remote patient monitoring.
Blood glucose monitors, activity trackers, and heart rate monitors are a few examples of wearable medical equipment. Improved patient engagement, expanded access to healthcare services, and enhanced precision in remote patient monitoring are all benefits of wearable technology for both patients and healthcare professionals. Additionally, wearable technology enables more individualized care and can aid healthcare professionals in making better choices regarding patient care. In general, wearable technology is an important telemedicine tool that can improve patient care and medical results.
Rural Areas and Telemedicine
Due to issues like scarce resources, a shortage of healthcare practitioners, and geographic barriers, access to healthcare services in rural areas of the United States is frequently extremely difficult. By making remote consultations, telemonitoring, and telehealth education possible, telemedicine can significantly contribute to enhancing access to healthcare in rural areas.
Telemedicine has already shown promise in enhancing rural residents’ access to healthcare. For instance, telemedicine has been utilized in Alaska to link patients in rural areas with specialists in urban areas, improving healthcare results and lowering costs. Similar to this, telemedicine has been used to deliver remote mental health services to underserved communities in rural Texas.
In conclusion, telemedicine has the ability to alleviate the problems with healthcare access that rural communities in the USA confront. Telemedicine can improve healthcare outcomes, lower healthcare costs, and improve people’ overall quality of life by offering remote healthcare services.
In the USA, there is a legal and regulatory framework for telemedicine.
In the USA, the telemedicine legal and regulatory environment is complicated and varies by state. Overall, state and federal regulations, as well as professional licensing bodies, control telemedicine. In light of the COVID-19 pandemic in particular, recent updates and modifications to telemedicine rules aim to expand patient access to healthcare services. In addition to loosened limits on telemedicine use across state boundaries, these developments have also increased remuneration for telemedicine services.
The acceptance and use of telemedicine are significantly impacted by legal and regulatory frameworks. To maintain compliance and prevent legal liability, healthcare organizations and providers must understand a complicated web of rules and regulations. However, a supportive regulatory framework can also promote innovation and investment in telemedicine, resulting in better patient outcomes and more access to healthcare services.
Conclusion
In summary, telemedicine has quickly become a vital part of the healthcare sector, particularly in the USA, where it has experienced substantial growth in recent years. The COVID-19 epidemic has advanced the use of telemedicine and highlighted the advantages of providing medical care remotely. This article has covered a number of important telemedicine topics, such as wearable technology, artificial intelligence, remote patient monitoring, teleconsultation, and the legal and regulatory environment in the USA.
The potential for telemedicine to increase efficiency, improve patient outcomes, and extend access to healthcare services are some of the main takeaways from this study. Additionally, telemedicine has proven that it may cut healthcare expenditures and cross geographical boundaries. The need for a supportive regulatory environment that promotes innovation and investment, as well as issues like maintaining patient privacy and data security, are obstacles that must be overcome.
The future of telemedicine in the United States is bright. The development of telemedicine and the transformation of how healthcare is provided in the nation are likely to be fueled by ongoing technological developments, increasing investment, and kind regulatory regulations.
Read More You May Like:








